How to Manage Periods Effectively with Mirena: What You Need to Know in 2025
The Mirena IUD (intrauterine device) has become a popular choice for women seeking effective birth control and menstrual management. Designed to gradually release hormones, Mirena not only prevents pregnancy but also impacts menstruation for many users. This comprehensive guide delves into how long it takes for Mirena to stop periods, the menstrual changes associated with Mirena, and everything you need to manage your menstrual health effectively with Mirena in 2025.
Understanding Mirena and Menstruation
The relationship between Mirena and menstruation is complex and varies from woman to woman. Many users seek Mirena for its contraceptive benefits, but its role in **menstrual regulation** cannot be overlooked. Knowing how Mirena affects periods is crucial for managing expectations. Typically, it may take about three to six months for users to notice the full effects, including significant changes in **period frequency and flow**. While some women experience lighter periods or sporadic bleeding, others may find that periods completely cease, a condition known as amenorrhea. Ongoing reviews highlight that **understanding individual responses** to Mirena is essential for effective management.
How Does Mirena Affect Periods?
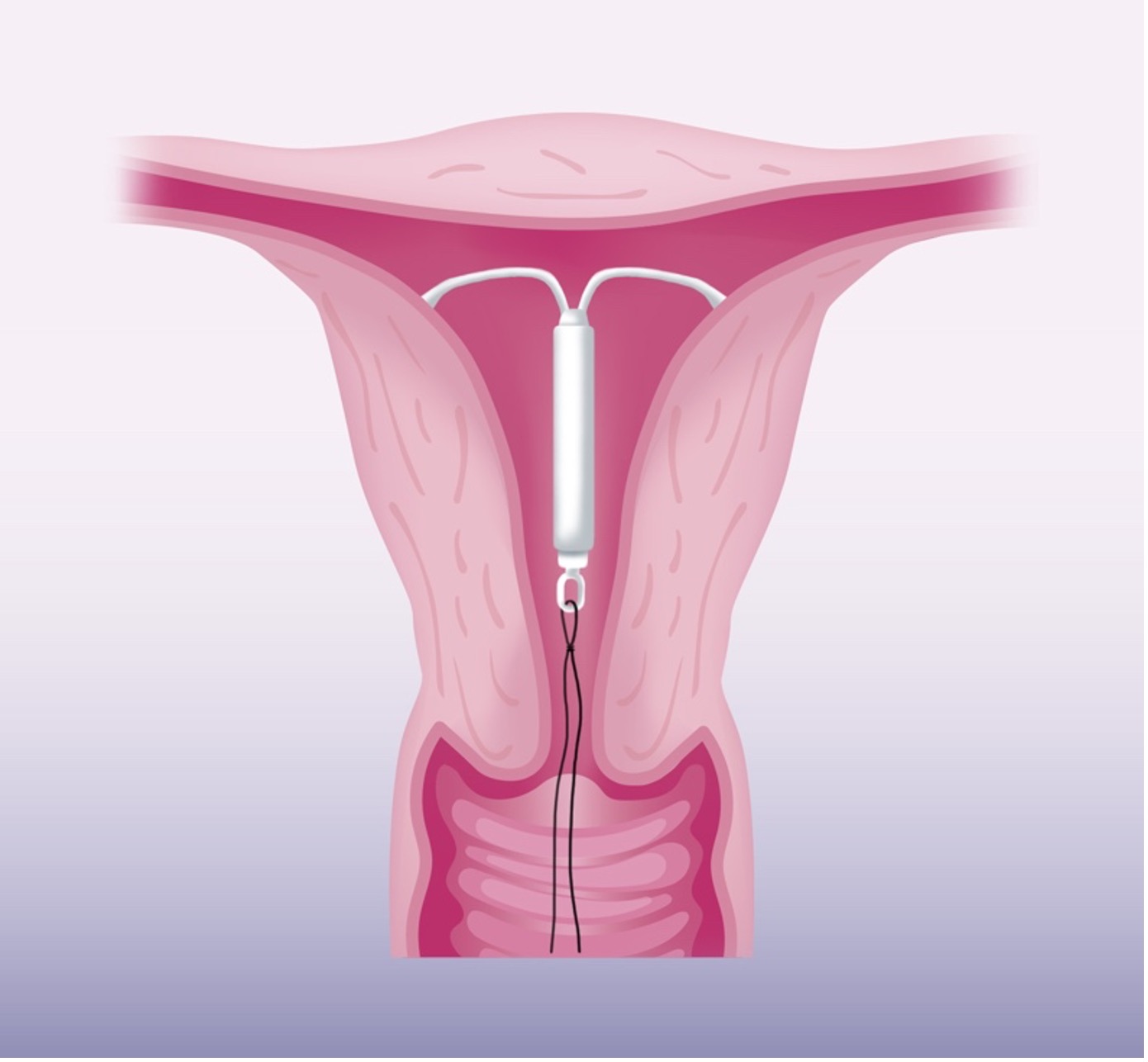
Mirena primarily releases the hormone levonorgestrel, which works to thin the uterine lining. As the lining becomes thinner, many users report **reducing periods with Mirena**, often leading to lighter menstruation or complete cessation. This hormonal manipulation can significantly alter the **menstrual cycle**. Some may experience intermittent periods termed “indeterminate periods” during the initial months. Understanding these effects helps users navigate the early adjustments and set realistic expectations about their **menstrual patterns**.
Mirena Insertion and Initial Period Changes
The **Mirena insertion process** can lead to temporary changes in menstrual cycles. Post-insertion, users may experience heavier bleeding or increased cramping as the body adapts to the IUD. Patience is key; during this adjustment, it is normal to see fluctuations in cycle length and flow. Engaging with healthcare professionals about potential impacts from the initial insertion can provide vital insights for managing period expectancy and aligning it with overall health goals.
User Experiences with Mirena and Menstruation
When discussing **Mirena user experiences**, one common theme emerges: **recognition of individual differences** in how Mirena affects menstruation. While many women appreciate reduced menstrual symptoms—such as less cramping and lighter flow—others might face challenges, including prolonged irregular bleeding in the early months. These firsthand accounts offer valuable lessons for those considering **Mirena as a birth control solution**. It’s beneficial for new users to connect with community forums and support groups to gather insights and learn from others’ journeys, helping to prepare them for their individual experiences.
Mirena Effectiveness and Usage Guidelines
Mirena is renowned for its effectiveness as a hormonal IUD. With proper placement and maintenance, it offers over 99% effective contraception and potential for **period control**. Knowing how Mirena works can empower users to maximize its benefits. This section will cover safety guidelines alongside **adjustments required** during Mirena usage, focusing on practicality and clarity.
How Mirena Works in Controlling Periods
Mirena’s primary mechanism revolves around its release of hormones, which act locally within the uterus. By thickening the cervical mucus and thinning the uterine lining, **Mirena effectively reduces bleeding** and cramping associated with menstruation. Additionally, feedback from **Mirena reviews** shows that many users experience substantial relief from heavy periods, marking it as an essential option in managing symptoms related to uterine conditions, such as fibroids. Understanding **Mirena treatment effects** allows users to appreciate its dual functionality of contraception and menstrual relief.
Mirena Maintenance and Check-Ups
Regular **check-ups** are crucial when utilizing a Mirena IUD. Healthcare providers recommend routine assessments to ensure proper placement and discuss any side effects or period changes. Users must stay vigilant for signs that might necessitate a consultation—such as experiencing sudden changes in flow after months of stability. Such proactive measures enhance the overall effectiveness of Mirena, allowing for ongoing dialogue about **side effects** and **hormonal balance** while using the device.
Blood and Bleeding Patterns with Mirena
One critical aspect worth noting is how Mirena influences **bleeding patterns**. Initially, users may notice an increase in spotting and irregular bleeding, especially in the first half of the year after insertion. However, as the body adjusts, many report significant reductions in menstrual flow overall. Understanding this **transition in bleeding patterns** not only eases user concerns but also highlights the importance of patience and consultation during this adjustment phase. Emphasizing open communication with healthcare providers can lead to better management of any complications that might arise.
Managing Side Effects and Expectations with Mirena
While many shrug off the **side effects of Mirena**, it’s essential to maintain awareness of potential changes and challenges. Users should be proactive in managing these effects and fostering discussions with their healthcare provider about their experiences. This section will cover navigating potential side effects while being aware of personal expectations surrounding menstruation with Mirena.
Adjusting Lifestyle with the Mirena IUD
Adjusting to life with Mirena may require minor lifestyle changes for optimizing **menstrual health**. Regular exercise, a balanced diet, and mindful stress management contribute significantly to **hormonal balance with Mirena**. Implementing self-care strategies ensures users maintain optimal health while minimizing potential side effects. Active discussions with doctors about individual health practices can assist in tailoring these changes effectively.
Managing Common Side Effects
Common side effects such as headaches, mood changes, and nausea can occur with Mirena usage. Being educated about these **side effects prevalence** can help users maintain control. Consulting with healthcare providers about symptom management and timelines can be tremendously helpful. Users must address concerns instead of delaying discussions, enhancing their overall experience with **the Mirena IUD**.
Consultation Before and After Insertion
Many women find it critical to engage in detailed discussions with healthcare providers both before and after insertion. Familiarizing oneself with **Mirena recommendations** and potentially necessary follow-up appointments enables proactive management of expected changes. These consultations can enlighten expectations surrounding side effects, period patterns, and even desired birth control outcomes.
Key Takeaways
- Mirena can significantly alter menstrual patterns, with many users experiencing lighter periods or even amenorrhea.
- Understanding the insertion process and subsequent adjustments is essential for effective period management.
- Regular check-ups and open communication with healthcare providers enhance the overall efficacy and comfort of using Mirena.
- Consumer experiences reveal diverse reactions, emphasizing the need for patience in adapting to the IUD.
- Lifestyle adjustments can complement the benefits of Mirena, ensuring greater control over menstrual health.
FAQ
1. How long does it take for Mirena to stop periods?
The timeline for how long it takes for **Mirena to stop periods** can vary. Most users may start experiencing changes after a few months, with significant improvements within six months of use. Some may achieve complete **period cessation with Mirena**, while others may notice lighter periods.
2. What are the common side effects of Mirena?
Common side effects include irregular bleeding, headaches, mood swings, and abdominal pain. While these can be concerning, most often they diminish within several months as the body adjusts to the hormonal changes and **effects of Mirena**. It is crucial to communicate any severe side effects to your healthcare provider.
3. Can Mirena be used for heavy periods?
Yes, Mirena can effectively treat heavy periods for many women. It works by thinning the uterine lining, which often leads to lighter menstrual bleeding. Those considering Mirena for **heavy periods** should consult with a healthcare provider about their options.
4. Are there any specific guidelines for using Mirena?
It is essential to follow doctor’s instructions regarding insertion and follow-up care. **Mirena usage guidelines** emphasize the importance of regular check-ups and self-monitoring for any side effects or unexpected changes in your menstrual cycle.
5. How does Mirena work as a hormonal birth control method?
Mirena works by gradually releasing the hormone levonorgestrel, which prevents pregnancy by thickening cervical mucus and thinning the uterine lining. This dual action contributes to its high effectiveness as a birth control method, in addition to managing menstrual health.